Effectiveness of Mindfulness Interventions on Neonatal Outcomes : A Systematic Review
DOI:
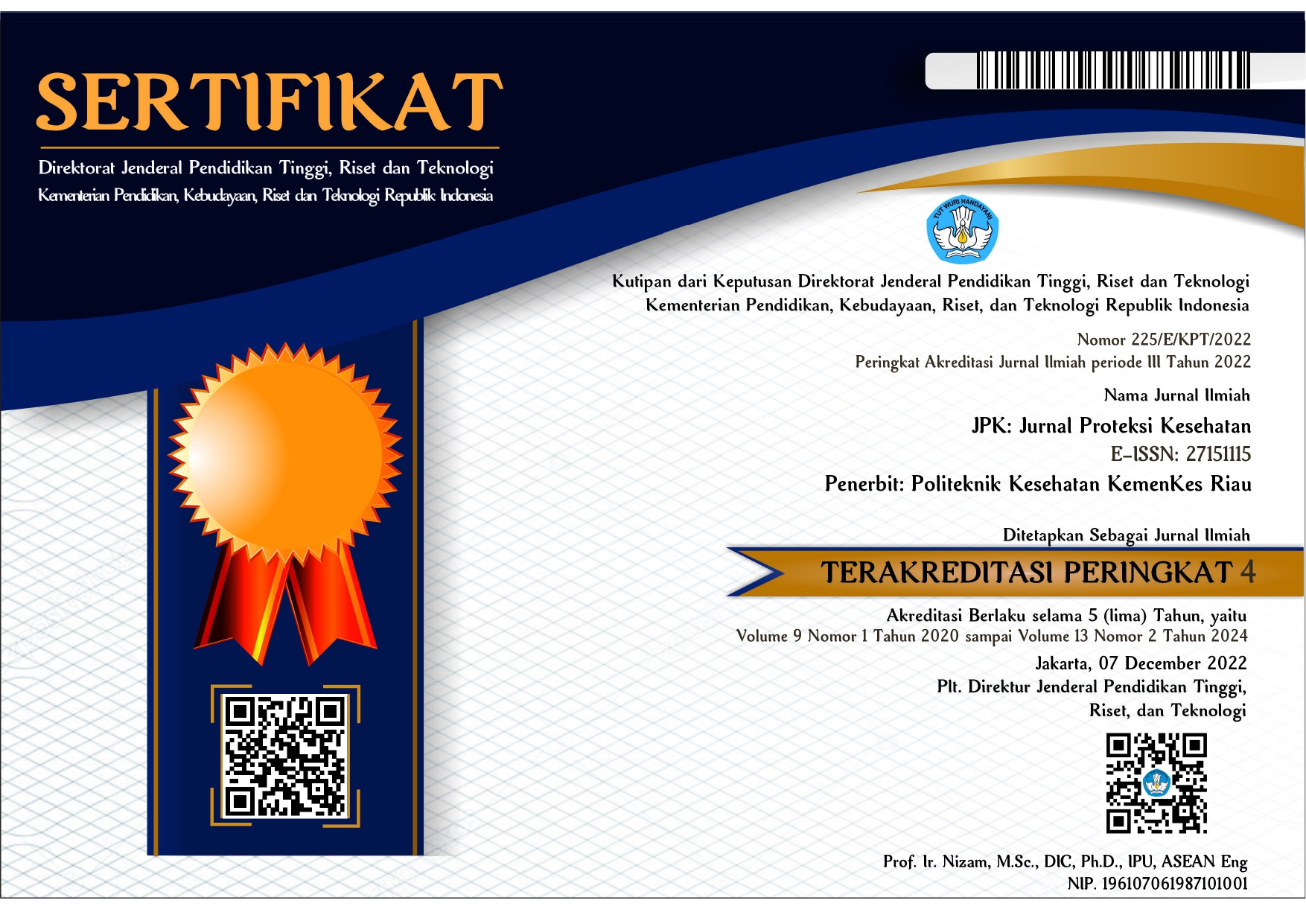
https://doi.org/10.36929/jpk.v12i1.648Abstrak
Abstract
Psychological stress during pregnancy is associated with negative birth outcomes, such as premature birth, low birth weight, gestational age at birth, indicators of breastfeeding, symptoms of postpartum depression, and can cause long-term defects in cognitive development. This study aims to determine the effectiveness of mindfulness interventions on neonatal outcomes through a systematic review. The method used in this study is a systematic review by searching articles through the Pubmed, ProQuest, Science Direct, Wiley Library, Sage Journal, and Cochrane Library databases with publication years January 2018 to January 2022. The results of the study obtained 6 articles that met the inclusion criteria, articles that discussed mindfulness on neonatal outcomes consisted of several countries, namely Canada, Egypt, the United States, San Francisco, Amsterdam, Netherlands. The use of mindfulness interventions for mothers with psychological distress suggests that mindfulness interventions are effective for improving labor outcomes and positive experiences during childbirth. From this study it can be concluded that mindfulness for the future can be used as a non-pharmacological intervention option to reduce psychological distress without risky side effects. Researchers suggest that further research is needed regarding the long-term effects after delivery and delivery outcomes.