Factors Affecting Early Detection of High Risk of Pregnancy
DOI:
https://doi.org/10.36929/jpk.v14i2.945Keywords:
Early detection, High Risk, PregnancyAbstract
Early detection of a high risk of pregnancy is crucial to prevent serious complications for the mother and fetus. However, the main challenge in pregnant women's health services in various regions is the low early detection rate. Factors such as education level, knowledge about pregnancy health, and access to health services are suspected to affect low awareness and preventive measures in pregnant women. This study aims to analyze the influence of these factors on the early detection of pregnancy risk using a cross-sectional quantitative approach with 103 pregnant women at the Tirto I Health Center, Pekalongan Regency, through a chi-square test. The findings showed a significant relationship between knowledge level (p-value 0.001), education (p-value 0.021), and health insurance ownership (p-value 0.017) on early detection of pregnancy risk. It is hoped that health workers can improve education and access to services to improve early detection of pregnancy risks.
References
[1] Kementerian Kesehatan Republik
Indonesia Direktorat Gizi dan
Kesehatan Ibu dan Anak, “Laporan
Akuntabilitas Kinerja Instansi
Pemerintah (Lakip) Direktorat Gizi Dan
Kesehatan Ibu Dan Anak Tahun
Anggaran 2022,” Jakarta:
Kementerian Kesehatan RI, 2023.
[2] S. Suparni, A. Fatkhudin, and N.
Zuhana, “Efektivitas Sibumil (Aplikasi
Deteksi Risiko Kehamilan Mandiri)
Berbasis Android Di Kota
Pekalongan,” J. Litbang Kota
Pekalongan, vol. 21, no. 2, p. 7, 2021,
doi: 10.54911/litbang.v21i1.163.
[3] DinKes Kabupaten Pekalongan, “Profil
Kesehatan Kabupaten Pekalongan
Tahun 2022.” Pekalongan:DinKes
Kabupaten Pekalongan, p. 74, 2022,
[Online]. Available:
https://drive.google.com/file/d/17g
gp2vYJSWrpwima5-
s5xNC_wcRNLt5Q/view.
[4] S. Khadijah and Arneti, “Upaya
Deteksi Dini Resiko Tinggi Kehamilan
Ditentukan oleh Pengetahuan dan
Dukungan Tenaga Kesehatan,” J. Sehat
Mandiri, vol. 13, no. 1, pp. 27–34,
2018, [Online]. Available:
https://jurnal.poltekkespadang.ac.id/
ojs/index.php/jsm/article/view/2/4.
[5] Kementerian Kesehatan RI, Buku
Kesehatan Ibu dan Anak. Jakarta:
Kementerian Kesehatan RI, 2019.
[6] L. D. Prafitri, W. Ersila, and D. Nurseptiani,
“Risk Factors for Carpal Tunnel Syndrome
in Pregnant Women,” J. Kedokt. dan
Kesehat. Indones., vol. 13, no. 1, pp. 52–
59, 2022, doi:
10.20885/JKKI.Vol13.Iss1.art9.
[7] Kementrian Kesehatan, Profil Kesehatan
Indonesia 2023. Jakarta : Kementerian
Kesehatan Republik Indonesia, 2024.
[8] WHO, “World health statistics 2022:
monitoring health for the SDGs,
Sustainable Development Goals,” World
Health Organization, 2022. [Online].
Available:
https://iris.who.int/handle/10665/3565
84.
[9] L. D. Prafitri, S. Suparni, and G. Setianto,
“Pendampingan Ibu Hamil Dalam Upaya
Deteksi Dini Resiko Tinggi Kehamilan,” J.
Community Dev., vol. 5, no. 3, pp. 423–
433, 2025, [Online]. Available:
https://comdev.pubmedia.id/index.php/c
omdev/article/view/287.
[10] E. P. Handayani, M. Jannah, and A.
Rahmawati, “Efforts To Increase Pregnant
Women’S Knowledge About High-Risk
Pregnancy With Health Education,”
Pharmacol. Med. Reports Orthop. Illn.
Details, vol. 1, no. 4, pp. 14–21, 2023, doi:
10.55047/comorbid.v1i4.591.
[11] D. R. Nainggolan and R. M. Ujung,
“Peningkatan Pengetahuan dan Deteksi
Dini Tanda Bahaya Kehamilan di Wilayah
Kerja Puskesmas Sipahutar Kabupaten
Tapanuli Utara Tahun 2022,” J. Mitra
Prima, vol. 4, no. 2, 2022.
[12] Z. Al Somali, E. Bajamal, and O. Esheaba,
“The Effect of Structured The Effect of
Structured Antenatal Education on
Childbirth Self-Efficacy,” Cureus J., vol. 15,
no. 5, 2023, doi: 10.7759/cureus.39285.
[13] E. C. De Araujo, N. Pereira, E. J. S. Tilman,
A. C. Da C, A. N. Corte, and R. Araujo,
“Effect of Reproductive Health Education
on Pregnant Women ’ s Knowledge about
Normal Delivery,” J. Int. Multidiscriplinary
Res., vol. 2, no. 5, pp. 450–462, 2024.
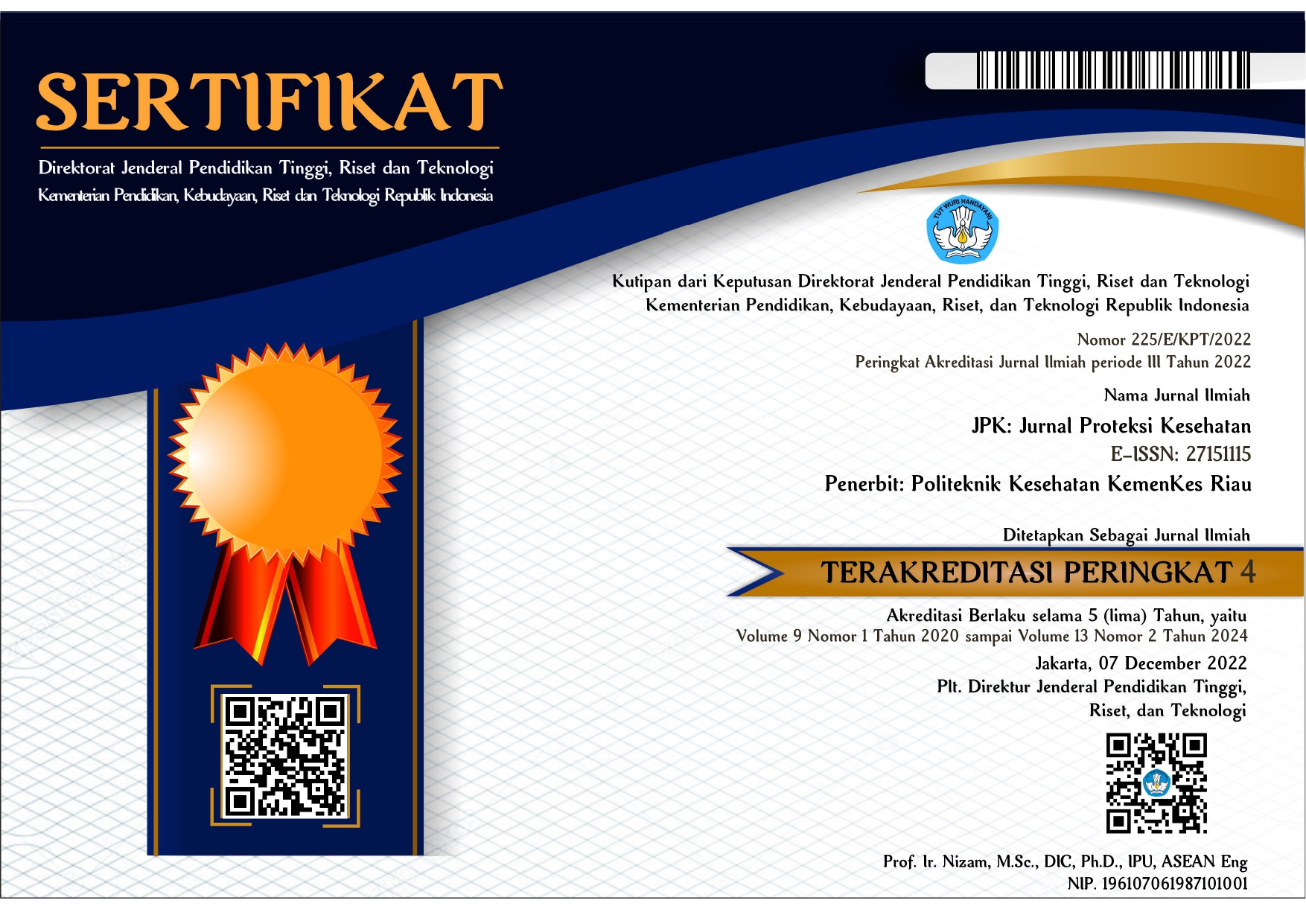
Jurnal Proteksi Kesehatan
Vol.14, No.2, November 2025, pp. 64-73
ISSN 2715-1115 (Online), ISSN 2302 – 8610 (Print)
Lia Dwi Prafitri and L02Prafitri@gmail.com 73
[14] S. Kamble et al., “Access, timeliness and
retention for HIV testing under early
infant diagnosis (EID) program, India,”
Sci. Rep., vol. 13, no. 1, pp. 1–11,
2023, doi: 10.1038/s41598-023-
32056-y.
[15] S. M. Alharbi et al., “Strategies to
improve the early detection and
management of ectopic pregnancies in
primary care,” Int. J. Community Med.
Public Heal., vol. 10, no. 7, pp. 2599–
2603, 2023, doi: 10.18203/2394-
6040.ijcmph20231772.
[16] B. P and S. Somashekar, “A Study on
Health Awareness During Pregnancy
with Special Reference to
Chamarajanagara District,” Int. J. Soc.
Heal., vol. 2, no. 6, pp. 391–396,
2023, doi: 10.58860/ijsh.v2i6.64.
[17] Fitriani, Sukri, S. Efendi, and N.
Sriyanah, “Early Detection of
Hypertension Symptoms in Pregnancy,”
Int. J. Community Serv., vol. 1, no. 2, pp.
142–147, 2022, doi:
10.55299/ijcs.v1i2.174.
[18] D. Feyisa, “Toward Universal Health
Coverage : The Role of Health Insurance,”
in Health Insurance, London: IntechOpen,
2022, pp. 1–14.
[19] H. A. Hamzah et al., “The Impact of Health
Insurance on Maternal Health Care in
Indonesia: A Systematic Review,” Research
Square, 2023.
https://doi.org/10.21203/rs.3.rs-
2855451/v1.
[20] N. F. Imamah, N. Ekadinata, G. Prayogo,
and B. A. Pramesona, “Employment,
Income, Health Insurance, Accessibility to
Healthcare Facility, Age, and Prenatal
Anxiety in Indonesia,” J. Aisyah J. Ilmu
Kesehat., vol. 8, no. 2, pp. 879–886, 2023,
doi: 10.30604/jika.v8i2.2046.
[21] X. Tao, Y. Zeng, S. Wang, J. Zheng, B. Ye,
and Y. Zheng, “Research on the impact of
medical and old-age security on the
utilization of medical services for the
disabled elderly,” Research Square, 2023.